Diagnostic Electrocardiography in Emergency Medicine
Introduction
Electrocardiography (ECG or EKG) remains one of the most essential and widely used diagnostic tools in emergency medicine. Its non-invasive nature, rapid acquisition, and rich diagnostic information make it indispensable for evaluating patients presenting with chest pain, palpitations, syncope, or other cardiac-related complaints. We will explore the critical role of diagnostic electrocardiography in emergency settings, highlighting its applications, interpretation, limitations, and advancements.
Definition
A Diagnostic Electrocardiograph is a medical device that records the electrical activity of the heart over a period of time, typically using electrodes placed on the patient’s skin. By capturing and displaying voltage fluctuations associated with each heartbeat, it generates an electrocardiogram (ECG) trace, which clinicians use to evaluate heart rhythm, detect abnormalities such as arrhythmias or ischemia, and guide diagnostic and treatment decisions.
What is Electrocardiography?
Electrocardiography is a diagnostic technique that records the electrical activity of the heart over time using electrodes placed on the skin. The depolarisation and repolarisation of the heart muscle with each beating cause minute electrical changes on the skin, which these electrodes pick up on. The recorded waveform, called an electrocardiogram (ECG), provides valuable insights into the heart’s rhythm, conduction system, and overall electrical function.
In emergency medicine, ECG is often the first-line diagnostic test for patients suspected of having cardiac problems because it offers quick and actionable information.
The Importance of ECG in Emergency Medicine
Early Identification of Life-Threatening Conditions:
If heart emergencies are not identified and treated quickly, they may be lethal. ECG is pivotal in detecting acute life-threatening cardiac conditions such as:
- Acute Myocardial Infarction (AMI): The classic ST-segment elevation myocardial infarction (STEMI) pattern on ECG is an emergency requiring immediate reperfusion therapy.
- Arrhythmias: Ventricular fibrillation, ventricular tachycardia, atrial fibrillation, and other arrhythmias can cause sudden cardiac arrest or hemodynamic instability.
- Electrolyte Imbalances and Drug Toxicity: Changes such as hyperkalemia or digoxin toxicity often manifest as specific ECG changes.
- Pericarditis and Pulmonary Embolism: These conditions may produce subtle but diagnosable ECG changes.
Early recognition via ECG allows for timely intervention, potentially saving lives and improving outcomes.
Guiding Treatment Decisions:
The management approach in the emergency department (ED) is immediately impacted by the results of the ECG. For instance:
- STEMI management: Identification of ST elevation triggers activation of the catheterization lab for urgent percutaneous coronary intervention (PCI).
- Arrhythmia management: The type and severity of arrhythmias determine whether electrical cardioversion, antiarrhythmic drugs, or pacing is needed.
- Risk Stratification: ECG abnormalities can help classify patients into low-, intermediate-, or high-risk categories for further monitoring or admission.
Monitoring Disease Progression and Treatment Effectiveness:
In the ED, serial ECGs can be crucial to detect dynamic changes that may indicate worsening ischemia or improvement after treatment. For example, ST-segment changes evolving over time can help assess myocardial injury progression.
Key ECG Parameters in Emergency Medicine
Emergency clinicians must be adept at recognizing critical ECG features. Important components include:
Heart Rate and Rhythm:
Determining whether the rhythm is regular or irregular and identifying the origin of the rhythm (sinus, atrial, junctional, ventricular) is foundational.
PR Interval, QRS Complex, and QT Interval:
- PR Interval: Prolongation may indicate heart block.
- QRS Complex: Widening suggests bundle branch block, ventricular rhythm, or pre-excitation syndromes.
- QT Interval: The risk of torsades de pointes, a severe ventricular arrhythmia, is increased by prolongation.
ST Segment and T Waves:
- ST Elevation: Suggests myocardial injury or infarction.
- ST Depression: May indicate ischemia or reciprocal changes.
- T Wave Changes: Inversion or hyperacute T waves can point to ischemia or infarction.
Pathological Q Waves:
These indicate past myocardial infarction.
Axis Deviation and Other Abnormalities:
Left or right axis deviation, ventricular hypertrophy, and conduction abnormalities add further diagnostic clues.
ECG Interpretation in Common Emergency Presentations
Chest Pain:
One of the most frequent reasons people visit the emergency room is chest pain. The main test used to distinguish between cardiac and non-cardiac causes is the ECG. Classic signs of acute coronary syndrome (ACS) on ECG include:
- ST-segment elevation (STEMI)
- New left bundle branch block (LBBB)
- T wave inversion and/or ST-segment depression (NSTEMI or unstable angina)
Prompt recognition enables rapid initiation of reperfusion therapy or other treatments.
Palpitations and Syncope:
In cases of palpitations or syncope, ECG can detect arrhythmias such as atrial fibrillation, supraventricular tachycardia, ventricular tachycardia, or heart blocks, guiding emergent interventions.
Dyspnea and Hypoxia:
Though often related to respiratory causes, some cardiac conditions like pulmonary embolism (PE) may show ECG signs such as sinus tachycardia, right heart strain pattern, or S1Q3T3 pattern, aiding diagnosis.
Limitations and Challenges
While ECG is invaluable, it is not without limitations:
- False Negatives: Early AMI or posterior infarctions may not show classic ECG changes.
- False Positives: Non-cardiac conditions can mimic ischemic ECG changes.
- Interpretation Variability: Skill and experience affect diagnostic accuracy; computerized interpretations should be confirmed by clinicians.
- Technical Issues: Poor electrode placement or patient movement can degrade signal quality.
Thus, ECG findings must always be integrated with clinical context and other diagnostic tests.
Advances in Electrocardiography for Emergency Medicine
Technology continues to enhance ECG utility in emergency settings:
- Portable and Wireless ECG Devices: Handheld ECGs facilitate early diagnosis even outside the hospital, e.g., in ambulances or remote areas.
- Continuous Telemetry Monitoring: Real-time ECG monitoring with remote access allows early detection of arrhythmias.
- Artificial Intelligence (AI): AI algorithms improve accuracy and speed of ECG interpretation, supporting clinicians under pressure.
- High-Resolution and Vectorcardiography: These provide more detailed cardiac electrical activity mapping.
Such innovations promise to improve diagnostic precision and patient outcomes further.
ECG Use Best Practices in Emergency Medicine
- Timely Acquisition: Obtain an ECG within 10 minutes for patients with chest pain or other suggestive symptoms.
- Proper Technique: Ensure correct electrode placement and patient preparation for accurate readings.
- Serial ECGs: Repeat ECGs to monitor evolving changes.
- Clinician Training: OED staff must get ongoing training in ECG interpretation.
- Integration with Clinical Assessment: Always correlate ECG findings with history, examination, and other investigations.
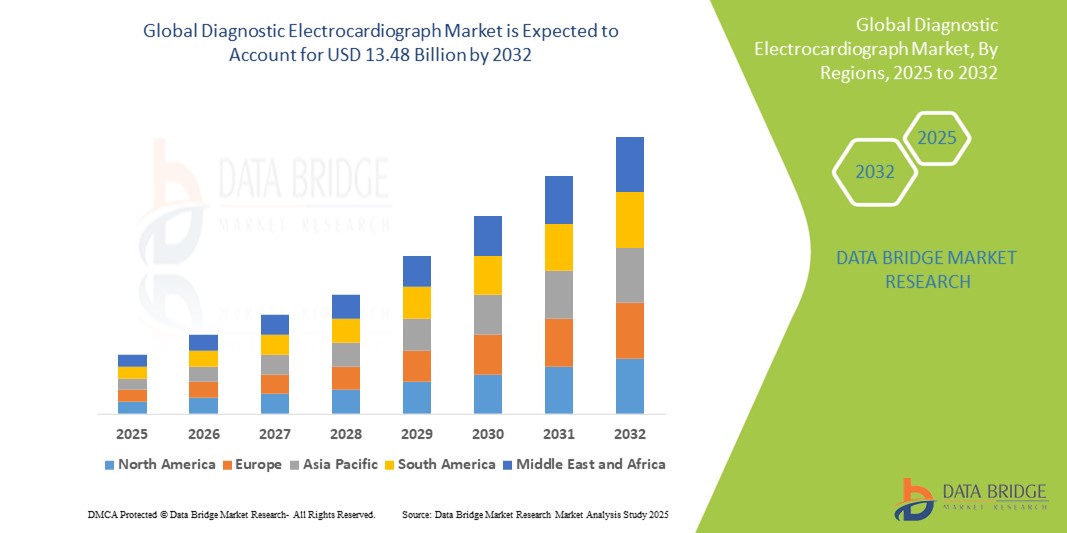
Growth Rate of Diagnostic Electrocardiograph Market
According to Data Bridge Market Research, the size of the global diagnostic electrocardiograph market was estimated at USD 8.84 billion in 2024 and is projected to grow at a compound annual growth rate (CAGR) of 5.41% to reach USD 13.48 billion by 2032.
Read More: https://www.databridgemarketresearch.com/reports/global-diagnostic-electrocardiograph-ecg-market
Conclusion
Diagnostic electrocardiography is a cornerstone of emergency medicine, crucial for early diagnosis, risk stratification, and management of acute cardiac conditions. Despite some limitations, its rapid availability, non-invasive nature, and rich diagnostic data make it indispensable in the emergency department.