Post-Vasectomy Pain: Myths vs. Mechanisms
A vasectomy is widely regarded as a safe, effective, and permanent form of male contraception. Despite its high success rate and minimal complication profile, a persistent concern among prospective patients and even some healthcare providers is the issue of post-vasectomy pain. This concern often stems from anecdotal reports, misinformation online, and a limited understanding of the underlying biological mechanisms.
In this article, we aim to dissect the myths surrounding post-vasectomy pain and explore the mechanisms that truly drive this condition, especially in cases of Post-Vasectomy Pain Syndrome (PVPS). By doing so, we offer both clarity and confidence to men considering this highly effective procedure.
Understanding the Basics: What Happens During a Vasectomy?
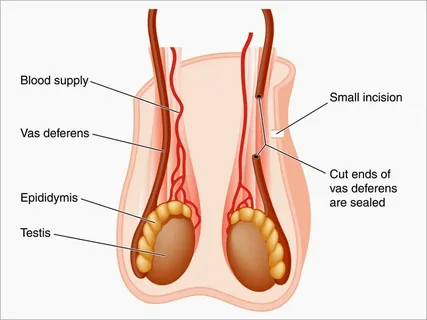
To grasp the cause of post-vasectomy pain, one must first understand the procedure itself. A vasectomy involves cutting or blocking the vas deferens, the tube that transports sperm from the testicles to the urethra. This blockage prevents sperm from mixing with semen during ejaculation, effectively rendering a man sterile.
Most vasectomies are performed in a urologist’s office under local anesthesia and take about 15–30 minutes. Common techniques include the conventional scalpel method and the no-scalpel vasectomy, which minimizes tissue trauma.
While recovery is generally quick, with most men returning to work within a few days, some report lingering discomfort that lasts for weeks, months, or in rare cases, years.
Myth 1: “Everyone Gets Chronic Pain After a Vasectomy”
One of the most pervasive myths is that chronic pain is a guaranteed consequence of vasectomy. In reality, most men experience only minor soreness for a few days post-procedure. The incidence of chronic pain—lasting more than three months—is estimated to be around 1–2%, and of those, only a fraction report pain that interferes with daily activities.
The majority of men resume normal sexual function and activity within a week or two. Therefore, portraying vasectomy as a procedure riddled with unavoidable chronic pain is medically inaccurate and unnecessarily fear-inducing.
Myth 2: “The Pain Is All in Your Head”
While some may dismiss post-vasectomy pain as psychosomatic, clinical evidence shows that in many cases, it is neuropathic or inflammatory in origin. Chronic pain after a vasectomy is a legitimate medical condition, and brushing it off as mere anxiety or expectation-induced discomfort undermines the experiences of men who suffer from it.
Research involving nerve conduction studies and testicular ultrasounds shows real physiological changes in men with persistent pain. These include nerve entrapment, sperm granulomas, and chronic inflammation—all well-documented causes of discomfort post-procedure.
Mechanism 1: Sperm Granulomas
Sperm granulomas are small, pea-sized lumps that form when sperm leaks from the cut end of the vas deferens into surrounding tissue. The body recognizes sperm as foreign, triggering an immune response that forms these granulomas.
In most cases, sperm granulomas are asymptomatic and even beneficial—they relieve back-pressure by providing a “release valve” for built-up sperm. However, in some men, they can become painful or inflamed, especially if they grow in size or compress nearby nerves.
Treatment may include anti-inflammatory medications, steroid injections, or surgical removal if the granuloma causes significant pain.
Mechanism 2: Congestion and Back-Pressure
Post-vasectomy congestion is another plausible mechanism. After the vas deferens is blocked, sperm production in the testicles doesn’t cease. The continuous generation of sperm can lead to back-pressure in the epididymis—the tightly coiled tube where sperm matures.
This pressure may lead to distension, inflammation, and discomfort. While some men naturally adapt over time through sperm reabsorption, others may experience prolonged irritation that manifests as a dull ache or pressure sensation, particularly after ejaculation.
Mechanism 3: Nerve Entrapment or Neuropathic Pain
Perhaps the most complex and challenging mechanism to treat is neuropathic pain, which stems from nerve injury or entrapment. During a vasectomy, even though care is taken to avoid nerve pathways, minor trauma to the genitofemoral, ilioinguinal, or pudendal nerves can still occur.
If scar tissue entraps these nerves, the result can be a sharp, burning, or radiating pain—distinct from the typical inflammatory or pressure-related discomfort. This type of pain often does not respond well to NSAIDs and may require more specialized treatment like nerve blocks or surgical denervation.
Diagnostic Approaches to Post-Vasectomy Pain
To determine the origin of post-vasectomy pain, physicians often rely on a combination of clinical history, physical examination, ultrasound imaging, and diagnostic nerve blocks.
- Physical Exam: Helps assess for tenderness, swelling, or masses like sperm granulomas.
- Ultrasound: Used to rule out conditions such as varicocele, hydrocele, or epididymal cysts.
- Nerve Blocks: Help determine if the pain is neuropathic and which nerve is involved.
This tailored approach ensures that the treatment aligns with the underlying cause rather than a one-size-fits-all pain management strategy.
Treatment Options: From Conservative to Surgical
Management of post-vasectomy pain depends on its severity, duration, and underlying cause:
Conservative Treatments
- NSAIDs: Often the first line of treatment.
- Scrotal support: To reduce mechanical strain.
- Ice therapy: Helps with inflammation in the initial days.
- Antidepressants or anticonvulsants: For neuropathic pain (e.g., amitriptyline, gabapentin).
Interventional Treatments
- Nerve blocks: Temporary relief for neuropathic pain and a diagnostic tool.
- Steroid injections: Reduce inflammation around granulomas or epididymis.
Surgical Treatments
- Sperm granuloma excision
- Epididymectomy: Removal of the epididymis.
- Denervation of the spermatic cord
- Vasectomy reversal: Can relieve back-pressure and congestion but is not guaranteed to eliminate pain.
Psychological Impact of Chronic Post-Vasectomy Pain
Chronic pain can have a significant emotional and psychological toll. Men may experience anxiety, depression, or sexual performance issues related to persistent discomfort. Unfortunately, because vasectomy is often framed as minor surgery, those experiencing prolonged complications sometimes feel dismissed or isolated.
Mental health support, alongside physical treatment, is crucial for comprehensive care. Cognitive-behavioral therapy (CBT) and patient support groups can offer valuable coping tools.
Preventing Post-Vasectomy Pain
While not entirely avoidable, certain practices reduce the risk of post-vasectomy pain:
- Choosing experienced surgeons: Reduces the chance of surgical error or nerve trauma.
- Minimally invasive techniques: Such as the no-scalpel method, reduce tissue damage.
- Proper post-op care: Includes scrotal support and avoiding strenuous activity.
- Patient education: Helps manage expectations and encourages early reporting of symptoms.
Real-World Perspective: What the Research Says
A 2022 study in the Journal of Urology followed over 1,200 men post-vasectomy and found that while 33% reported some pain in the first two weeks, only 1.8% reported persistent discomfort at six months. Of those, only 0.4% required surgical intervention.
This reinforces that vasectomy is a low-risk procedure with a high satisfaction rate—but awareness of complications allows for quicker diagnosis and effective management when things don’t go as expected.
Final Thoughts
Pain after a vasectomy, though rare, is real and multifaceted. The myths that overstate or understate its prevalence are harmful. Understanding the physiological mechanisms—like sperm granulomas, back-pressure, and nerve entrapment—enables more accurate diagnoses and targeted treatments.
Men considering a vasectomy should be informed, not frightened. With skilled providers and proper post-operative care, the vast majority of patients recover quickly and go on to enjoy the benefits of permanent contraception with minimal complications.
FAQs
1. Is post-vasectomy pain permanent?
No, most post-vasectomy pain resolves within a few days to weeks. In rare cases, chronic pain may last longer, but only about 1–2% of men experience this. Treatments are available depending on the cause of the pain.
2. Can vasectomy reversal cure post-vasectomy pain?
Yes, in some cases. If pain results from back-pressure or congestion, vasectomy reversal can relieve symptoms. However, it is not always effective, especially if the pain is nerve-related.
3. How can I lower my risk of post-vasectomy pain?
Choose a skilled urologist, follow all post-op instructions, wear scrotal support, and avoid strenuous activities. Early treatment of symptoms like swelling or lumps can also prevent complications